Hormonal health
Les Mills launches toolkit to help women stay active throughout their menstrual cycle
Menstruation can make it tough to maintain training habits, with 79 per cent of women skipping workouts when their period starts

Les Mills has launched a free toolkit to help women stay active and get the most from workouts throughout their menstrual cycle.
The world leader in group training has designed a series of workouts and educational resources to navigate the physical and mental effects of the menstrual cycle, guided by the principles of “cyclical training”.
The impact of menstruation on training is far-reaching and significant. Three-quarters of female athletes suffer negative side effects based on their cycle – a figure thought to be even higher among non-athletes – while 79 per cent of women take a day off exercise when their period starts.
Cyclical training helps women tailor their training schedule to match the different phases of hormonal activity throughout the month. The technique, Les Mills argues, could support stable training habits before, during and after menstruation, as well as unlocking the hidden benefits.
“We want to make it easy for people to adjust their training and nutrition throughout the menstrual cycle,” said Les Mills chief creative officer Dr Jackie Mills, a nutrition specialist and former obstetrician.
“Understanding the influence your cycle has will allow you to unleash your full potential and really get the most out of your training. It’s going to make things so much better for your mind and your body.”
The menstrual cycle is divided into two phases, the follicular and luteal, with each having unique effects on the body. Les Mills presenter and cyclical training fan Kaylah-Blayr Fitzsimons-Nu’u says the oestrogen spike that occurs in week two makes it the perfect time to crank things up.
“I feel really strong. I train heavier with my weights and add in a LES MILLS Sprint or GRIT. I’ve even found myself able to increase my chin-up PBs on week two,” she explained.
She’s equally philosophical about the days she has to taper her training to be kinder to her body and mind, noting that the focus should be on movement.
“It’s all about adjusting the intensity to suit the day of your cycle,” the presenter added.
“The great thing about cyclical training is it’s so intuitive. You reap the endless benefits of being active, while staying kind to yourself and attuned to your body’s needs as you progress through the month.”
The full range of cyclical training workouts is free to access on the LES MILLS+ streaming platform.
News
NHS health checks to include menopause questions for the first time

NHS health checks will include questions about menopause for the first time, a move ministers say could help up to five million women in England.
The Department of Health and Social Care said the new questions, to be developed over the coming months, could be introduced from 2026.
Adults aged 40 to 74 without long-term conditions are eligible for these free checks every five years.
The checks currently screen for heart and kidney disease, type 2 diabetes, dementia and stroke risks.
Adding menopause questions marks what health secretary Wes Streeting described as giving women “the visibility and support they have long been asking for.”
Streeting said: “Women have been suffering in silence for far too long.
“They are left to navigate menopause alone, with very little support – all because of an outdated health system that fails to acknowledge how serious it can be.
“No one should have to grit their teeth and just get on with what can be debilitating symptoms or be told that it’s simply part of life.”
Around three-quarters of women experience symptoms such as hot flushes, night sweats, depression and sleep problems.
One in four describe their symptoms as severe.
National Institute for Health and Care Excellence guidance recommends hormone replacement therapy (HRT) as the first-line treatment. HRT can also help maintain muscle strength and reduce the risk of osteoporosis, where bones become weak and brittle.
Despite this, many women say they are not listened to or offered adequate support.
Dr Sue Mann, NHS England’s national clinical director for women’s health, said: “By tailoring NHS health checks to include questions around menopause, we hope more women will get the support they need to manage their symptoms.”
Experts welcomed the move but cautioned that access inequalities remain.
Professor Ranee Thakar, president of the Royal College of Obstetricians and Gynaecologists, called it “fantastic news” that could help reduce stigma, but said implementation would be key.
“For this change to have maximum positive impact we’d like to see a real focus on ensuring women from diverse ethnic communities and socially deprived areas are supported to access health checks, and excellent menopause training for healthcare assistants providing them,” she said.
Kate Muir, author of Everything You Need to Know About the Menopause (But Were Too Afraid to Ask), said: “This is desperately needed, particularly to provide evidence-based information for women on the benefits of HRT. GPs’ appointments are a perfect way to get knowledge into all communities.
“We know from NHS statistics that 23 per cent of white menopausal women are on HRT, but only 5 per cent of black and 6 per cent of Asian women.
“This may open doors.”
Janet Lindsay, chief executive of Wellbeing of Women, added: “Women and people from marginalised communities are less likely to know about or attend these [health checks], and progress on menopause support cannot leave them behind.
“Healthcare professionals must work with grassroots organisations in these communities to ensure those facing additional barriers receive the tailored care they need.”
News
Women better protected against early Parkinson’s neurodegeneration, study finds
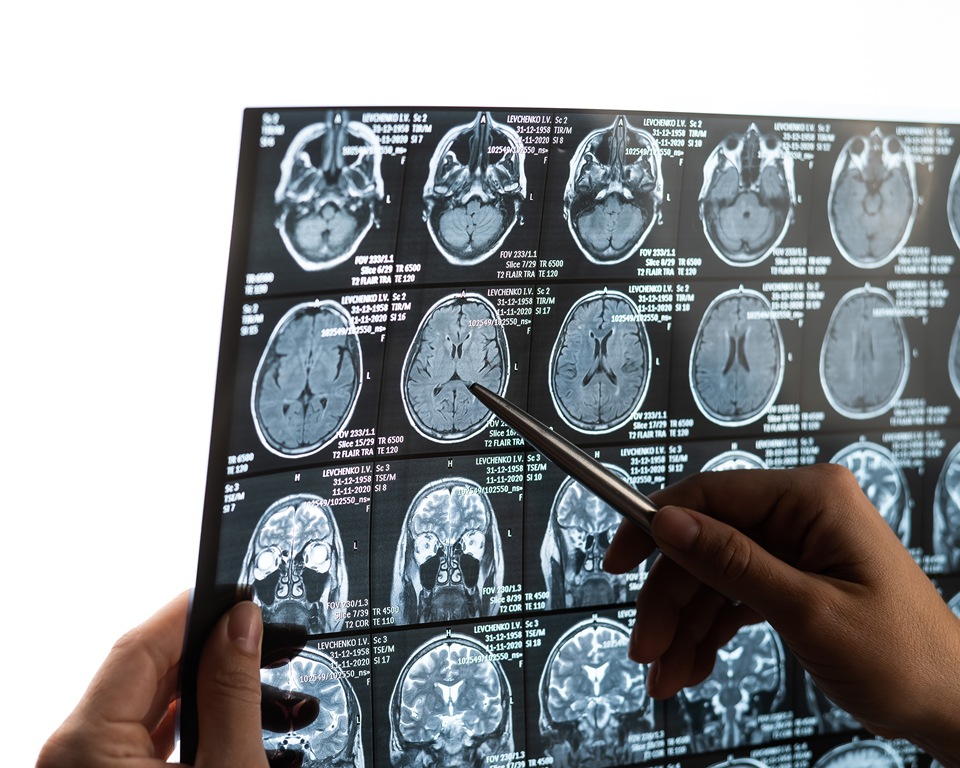
Women with an early precursor to Parkinson’s disease show much less brain shrinkage than men, despite similar disease severity, new research shows.
The discovery could help scientists explore how hormones might one day be used to treat the neurodegenerative condition.
The findings are based on data from nearly 700 participants across nine international research centres.
The study focused on isolated REM sleep behaviour disorder — a condition in which people physically act out their dreams.
It is considered the most reliable early warning sign of diseases caused by toxic protein build-up in the brain.
More than 70 per cent of those affected later develop Parkinson’s disease, Lewy body dementia or multiple system atrophy, which affects several body systems.
Researchers from Université de Montréal analysed 888 brain scans from centres in Canada, the Czech Republic, the UK, France, Australia, Denmark and Italy.
After quality checks, 687 participants were included: 343 patients with the sleep disorder and 344 healthy controls.
The results revealed clear sex-based differences.
While 37 per cent of the cortical areas — the brain’s outer layer responsible for higher functions — showed thinning in men, only one per cent of regions were affected in women.
This difference remained even though participants were of similar age (around 67) and had comparable clinical profiles.
Marie Filiatrault is first author of the study and a doctoral student at Université de Montréal.
The researcher said: “Men show much more extensive and severe cortical thinning — the outer layer of the brain that controls our higher functions — than women, particularly in areas linked to movement, sensation, vision and spatial orientation.”
To understand the protective effect, researchers compared brain images with gene activity in different regions, measured in healthy brains after death.
They found that the less-affected areas in women showed higher expression of genes related to oestrogen function, particularly ESRRG and ESRRA, which produce oestrogen-related hormone receptors.
The ESRRG gene was especially notable, showing greater activity in brain tissue than elsewhere in the body.
These receptors play key roles in mitochondrial function — the cell’s energy production system — and in the survival of dopamine-producing neurons, the cells that die in Parkinson’s disease.
Shady Rahayel is professor at Université de Montréal’s Faculty of Medicine and lead author of the study.
Rahayel said: “This sleep disorder offers a unique window of opportunity to study the mechanisms of neurodegeneration before major motor or cognitive symptoms appear.
“Our results suggest that certain brain areas in women with isolated REM sleep behaviour disorder are better protected than those in men, likely through the action of oestrogens.”
The team chose to study this precursor condition because it allows observation of brain protection mechanisms before major motor symptoms develop.
Although only 25 to 40 per cent of people with Parkinson’s experience REM sleep behaviour disorder, studying this early stage gives insight into how the brain resists damage when it is still limited.
Previous studies have shown that women with established Parkinson’s disease tend to experience slower progression than men, pointing to similar protective effects.
The findings could shape future research and treatment development.
The authors recommend separating men and women in clinical trials, which could improve statistical accuracy and reduce the number of participants required.
The biological mechanisms identified — particularly those linked to the ESRRG gene — could also become potential therapeutic targets.
Early laboratory research suggests that increasing ESRRG activity may protect dopamine-producing neurons from the toxic effects of alpha-synuclein, a protein that builds up abnormally in the brains of people with Parkinson’s.
“This study brings us closer to precision medicine, where treatments could be tailored not only to the disease but also to individual biological characteristics, including sex,” said Rahayel.
Hormonal health
Dozens of women report suffering painful burns after using Always sanitary towels

Dozens of women have claimed online that Always sanitary towels caused painful burns, prompting a response from the Procter & Gamble-owned brand.
Several TikTok users have posted videos describing reactions to the company’s products in recent days.
The clips, which have gained thousands of views, include complaints of itching, rashes and what users describe as chemical burns — skin damage caused by contact with irritating substances.
In one video viewed 45,000 times, user @ratqueen910 said the pads gave her “the worst chemical burns ever” in her groin area, where underwear meets the leg.
“When I looked at the burn with the flash on it really looked like my skin was gooey! I was scared af,” she told commenters.
She said she first thought the pain was chafing or an allergic reaction to spandex in her underwear, before seeing other women online describe the same symptoms.
“I realised that so many people have had problems the last few months with these pads,” she said.
“It’s not like, ‘oh, I switched over to Always pads’ — no, I’ve used them since I was in like sixth grade.
“So they must have changed the formula, messed something up, put some extra chemicals in that sh**t because it messed me up. I had chemical burns. I had issues and I didn’t know what it was.”
She said a doctor suggested another cause for the irritation, but she believes the pads were to blame, noting she had never been sensitive to scents or suffered urinary or yeast infections before.
Her post drew hundreds of comments, with many women saying they too had reactions to Always’ Flexfoam pads.
One wrote: “The whole area that the pad touched gave me a chemical burn after only a few hours. It was the Flexfoam.”
The original poster replied: “Mine was Flexfoam as well.”
While users did not specify exact product types, Always sells both day and night versions of its Infinity Pads with Flexfoam, which appear to be those mentioned.
Another commenter said: “Just a few days ago I was on my period using Always pads and I was f**king itching and it was burning. I never itch or have pain down there. I took the pad off so quick.”
A third wrote: “I switched to Honey Pot and had been fine. When my coworker gave me an Always pad, I was hesitant but used it — and got a chemical burn.”
Others described repeated irritation.
One said: “I use another brand for the first half of my period, then Always for the last two days, and I’ve had this burn for three months in a row. Stopped using them last month and no issue.”
Some also reported rashes or itching. One wrote: “In real time I am itching and getting a rash. I wore an Always pad earlier today.”
An Always spokesperson told the Daily Mail: “Our pads are used safely by millions of women every day around the world.
“Their safety is our top priority, and we carefully evaluate every component of our Always products to minimise the chances of skin irritation or allergic reactions.”

 Hormonal health20 hours ago
Hormonal health20 hours agoDozens of women report suffering painful burns after using Always sanitary towels

 News2 weeks ago
News2 weeks agoFDA plans to revise black box warning on menopause hormone therapies

 News2 weeks ago
News2 weeks agoAI-powered women’s health companion Nexus launches in UK

 News2 weeks ago
News2 weeks agoScientists turn human skin cells into eggs in IVF breakthrough

 News7 days ago
News7 days agoWomen’s health innovations recognised in TIME’s Best Inventions 2025

 Hormonal health2 weeks ago
Hormonal health2 weeks agoDaily pill could delay menopause ‘by years,’ study finds

 News2 weeks ago
News2 weeks agoAncient herb to modern must-have: Why ashwagandha is capturing UK women’s attention

 Menopause3 weeks ago
Menopause3 weeks agoNew report exposes perimenopause as biggest blind spot in women’s health