Fertility
Why we need to prioritise early fertility support
Early intervention and emotional support matter, say Lucy Buckley and Kobi McCardle

Fertility treatment can be an emotional rollercoaster. We sat down with Lucy Buckley and Kobi McCardle, co-founders of the online platform Dr Fertility, to find out why we need to do more for those unable to conceive.
Depending on the area where you live in, getting fertility treatment following a GP referral can take any time between 21 weeks and two years. Despite such discrepancies, six out of every 10 IVF cycles are still funded privately.
“A lot of the time, these couples feel in limbo,” says Lucy Buckley, clinical pharmacist and co-founder of Dr Fertility, an online platform for personalised fertility support, tests and prescriptions.
“With so much misinformation, it’s easy to self-diagnose and jump to conclusions,” Buckley insists. “So, with our platform we wanted to show the importance of seeking support from the very beginning instead of waiting until you’re struggling.”
Her co-founder, Kobi McCardle, agrees. Although fertility declines with age, negative lifestyle and diet choices can also impact women’s chances of getting pregnant.
“Fertility support is more needed now than ever,” McCardle says. “When we look at the statistics, we can see that couples consider starting a family much later in their life and about 50 per cent of women born in the 1990s still don’t have children.
“So, we’re very focused on supporting people right from the start and ultimately, reducing the number of couples having to undergo IVF.”
The two founders think that this also comes down to education. Programmes like the Fertility Education Initiative (FEI), a special interest group of the British Fertility Society, aims to improve knowledge of reproductive health in young people who will likely know little about factors that could lead to infertility.
“We’re now seeing how younger generations are becoming much more proactive in terms of their health care and we’ve had couples in their early 30s who just wanted to make sure that everything was okay,” Buckley explains.
“But although we’re seeing this change in mindset, we need to do more in terms of fertility education. We’ve got some great educational content on our website and we really hope to help in that regard.”
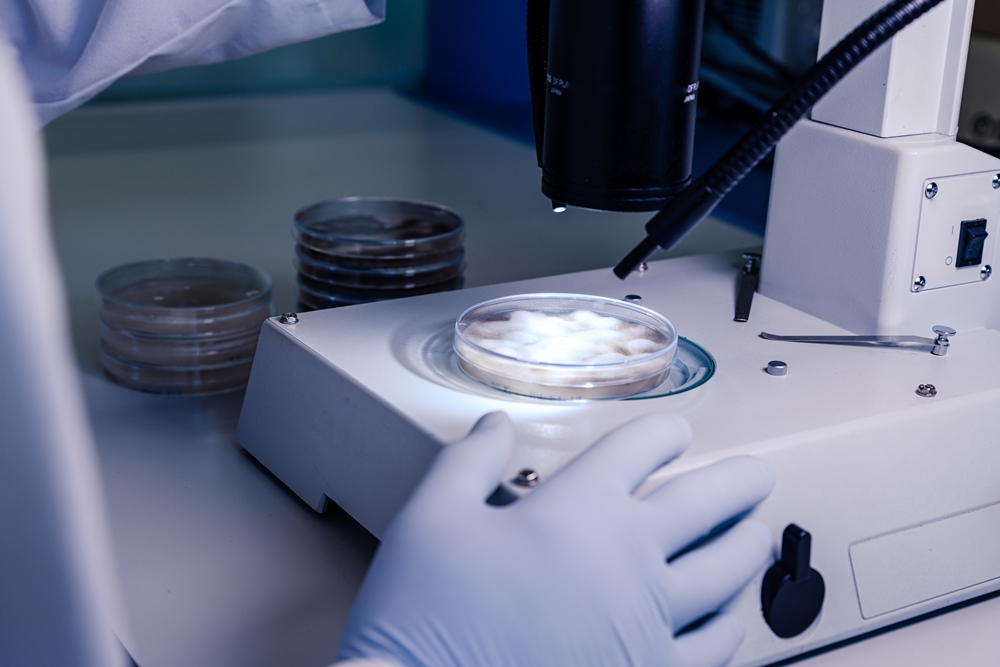
Dr Fertility is regulated by the Care Quality Commission and offers medical and emotional support through the provision of accessible online advice, diagnostic testing, blood testing, treatment and coaching from home.
“We don’t just look at the medical elements,” Buckley adds. “We look at the couple’s emotional status, lifestyle and social situation and provide ongoing support.
“We are very passionate about helping people. Fertility is such an emotional topic and it’s that emotional support that matters the most.”
Although an increasing number of people go through fertility treatment, showing the value of talking to a fertility expert has not been easy for the two founders.
“That and finding the right people have proved more challenging than we thought,” McCardle adds. “In a digital health start-up like this, you’ve got people coming in from lots of different industries and with lots of different backgrounds, but now we’re happy to have a great team behind us.”
Along with improving the platform, the two founders hope to extend their services in the UK market and to provide further support for people throughout their fertility journey.
“Early intervention is extremely important,” says Buckley. “If there is an issue we want to know earlier on so we can do everything we can to support our patients.”
For more information, visit drfertility.co.uk.
News
Patients take legal action to save frozen embryos after admin error
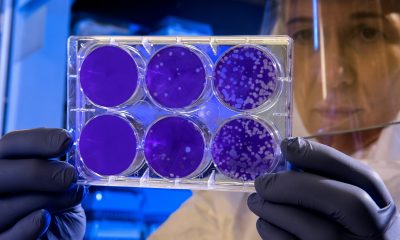
At least 15 fertility patients are taking legal action to prevent their frozen embryos being destroyed after administrative errors left them at risk of losing their chance to have children.
The group includes people with cancer and fertility problems who froze gametes (eggs and sperm) or embryos to improve their chances of conceiving later on, but were told they had not renewed consent in time due to clinic mistakes.
Some only discovered the problem when they approached clinics about plans to start a family — for some, their only hope of conceiving naturally.
Others were contacted by clinics after internal audits revealed the errors and were told they could only extend storage through a court order.
The errors relate to two legal changes: one in 2022 that extended the maximum storage period for embryos and gametes from 10 to 55 years for personal use, provided consent is renewed every 10 years; and a temporary two-year extension introduced during the coronavirus pandemic in 2020.
In several cases, clinics failed to contact patients about renewing consent, recorded incorrect expiry dates or medical details, or did not follow up on reminders.
Some patients missed emails that did not make the urgency clear, while others continued to make annual storage payments, assuming everything was in order.
James Lawford Davies, a partner at LDMH Partners representing the group, said that although the fertility law change had been “positive and well intentioned”, both clinics and patients had found the new rules “difficult to understand and apply.”
He said: “The cases before the court have arisen as a result of errors, oversights and misunderstandings surrounding the new rules.
“The applications are hugely significant for all the patients involved and, for many, this represents their only chance of having their own genetic child.
“We hope that, going forward, the guidance and process for storage consents can be clarified and simplified for patients and clinics alike.”
Appearing in the high court this week, Emma Sutton KC, representing the applicants, said they felt “emotional” and “distressed” as they “would have given their consent had the process been put into effect in the way it should have.”
She added that the patients had been left “in limbo” for nearly a year, with “time of the essence” for some couples because of age or health problems.
She argued that destroying the embryos would conflict with article 8 of the Human Rights Act, which gives people the right to a family life, and said allowing extensions “would not undermine a fundamental objective of the statutory scheme – namely the requirement for consent.”
Barristers representing the Human Fertilisation and Embryology Authority (HFEA) and the Department of Health and Social Care supported case-by-case consideration and proposed that, where clinics failed to notify people, patients should be given six months to arrange consent renewal.
Jeremy Hyam KC, for the Department of Health and Social Care, expressed concern that the law’s focus on effective consent could be undermined if there were a “free for all”, leading clinics to adopt a “default position of indefinite storage” out of fear of liability for miscommunication.
He said cases in which patients had been notified but made errors — such as failing to open emails, update addresses or log into online portals — should not automatically be granted extensions.
Ravi Mehta, for the HFEA, expressed the regulator’s “sympathy” for the patients and praised clinics for their “candour” in admitting mistakes.
He noted that under UK fertility law, clinics — not patients — are responsible for securing consent.
“[The patient’s] wishes now are sufficient – no one is asking for open-ended relief, that takes consent now as opening the door to everything.”
Mrs Justice Morgan, who heard the case, will deliver a written judgment in the coming months.
Diagnosis
Morning-after pill now free across pharmacies in England

The NHS has made the morning-after pill free at almost 10,000 pharmacies in England, ending postcode lottery access to emergency contraception.
Women can now obtain the emergency pill without charge at their local pharmacy, removing the need to visit a GP or attend a sexual health clinic. Some pharmacies had previously charged up to £30 for the service.
The NHS described the rollout as “one of the biggest changes to sexual health services since the 1960s.”
Dr Sue Mann, the NHS’s national clinical director for women’s health, said the expansion was “a gamechanger in making reproductive healthcare more easily accessible for women.”
She said: “Instead of trying to search for women’s services or explain their needs, from today women can just pop into their local pharmacy and get the oral emergency contraceptive pill free of charge without needing to make an appointment.
“With four in five people living within a 20-minute walk from a pharmacy, this service is another example of how the NHS is already delivering on our 10-year health plan commitment to shift care into the heart of communities.”
The announcement coincides with the NHS expanding pharmacy services to include support for people newly prescribed antidepressants, who can now seek advice and guidance about their medication and healthy lifestyle changes from their local pharmacist.
Henry Gregg, chief executive of the National Pharmacy Association, which represents about 6,000 independent pharmacies across the UK, welcomed the change.
He said: “We’ve long called for the national commissioning of emergency contraception so this is good news for patients and pharmacies alike that this is launching today.
“For too long, access to free emergency contraception has been a postcode lottery for patients, with local arrangements only existing in certain parts of the country.
“It’s really important that pharmacies, which are under significant pressure and closing in record numbers, are sustainably funded so they can continue to provide services to patients such as these.”
Stephen Kinnock, minister for care, said: “This is a major step forward that removes barriers of access to reproductive care that have let women down for too long.
“Pharmacies play a central role in communities, trusted by local people and easy to access. That’s why it’s vital there are a wide range of services and medications available.”
News
AI embryo selection tool wins European approval
Alife Health’s AI-powered embryo selection software has received CE Mark certification under the European Medical Device Regulation (MDR), allowing it to be used in fertility clinics across Europe.
The San Francisco-based company said its Embryo Predict system, which supports embryologists in selecting the best embryo for transfer, can now be marketed across EU countries following MDR approval.
The software uses deep learning – a type of artificial intelligence that mimics how the brain processes information – to help embryologists assess embryos during IVF.
It captures embryo images, generates an AI score and ranks them according to their likelihood of resulting in a clinical pregnancy.
Traditional embryo assessment relies on manual observation of embryo morphology – the study of its shape and structure – which can vary between embryologists.
The AI tool aims to standardise this process by analysing large datasets and detecting subtle patterns beyond what the human eye can identify.
Melissa Teran, CEO of Alife Health, said: “Achieving CE Mark approval is a significant step in our mission to improve patient outcomes and expand access to fertility care.
“With Embryo Predict now available to clinics across Europe, we have moved one step closer to our goal of achieving global impact in reproductive medicine.
“We look forward to partnering with leading IVF centres across Europe to bring the benefits of AI to more patients.”
With MDR clearance secured, Alife plans to roll out Embryo Predict to selected IVF clinics across the EU, building on its existing momentum in the US, where it operates a clinical decision support platform and partners with leading fertility networks.
Alife Health develops AI-driven tools to modernise and personalise IVF.
The company has not disclosed pricing for the European market or timelines for individual country launches.
Dr Marcos Meseguer is global director of embryology research at IVIRMA, who is collaborating with Alife on innovative embryo research sponsored by the European Council.
Meseguer said: “I was impressed not only by Embryo Predict’s precision in scoring embryos, but also by the simplicity of its integration with existing laboratory hardware.
“Alife brings a level of standardisation and objectivity to embryo selection that our field needs.
“By combining human expertise with AI-driven insight we will reduce subjectivity and improve decision-making.”

 News1 week ago
News1 week agoDozens of women report suffering painful burns after using Always sanitary towels

 News4 weeks ago
News4 weeks agoFDA plans to revise black box warning on menopause hormone therapies

 Insight2 weeks ago
Insight2 weeks agoWomen’s health innovations recognised in TIME’s Best Inventions 2025

 Entrepreneur3 weeks ago
Entrepreneur3 weeks agoAI-powered women’s health companion Nexus launches in UK

 News4 weeks ago
News4 weeks agoScientists turn human skin cells into eggs in IVF breakthrough

 News2 weeks ago
News2 weeks agoCutting through the noise in femtech – key takeaways from Women’s Health Week 2025

 News3 weeks ago
News3 weeks agoMenstrual cycle affects women’s reaction time, study finds

 Menopause4 weeks ago
Menopause4 weeks agoDaily pill could delay menopause ‘by years,’ study finds





























1 Comment